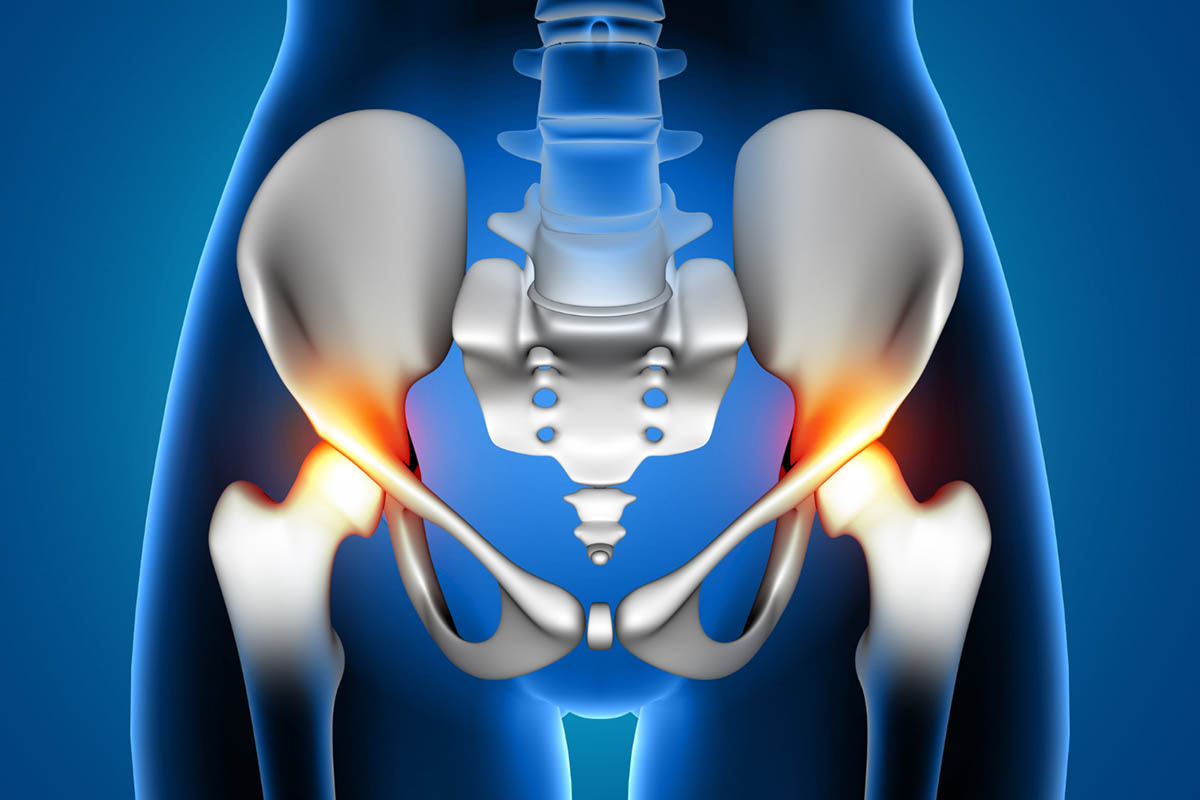
Lower back and pelvic pain are common issues faced by many women, impacting their daily lives and overall well-being. Most people experience LBP at some point in their lives. The peak in the number of cases occurs at 50–55 years, and women experience LBP more frequently than men. These conditions can range from mild discomfort to severe pain, and their effects can significantly affect daily activities and quality of life. This article will explore the causes, symptoms, diagnosis, and treatment options for females’ lower back and pelvic pain, providing a comprehensive overview to help manage and alleviate these common issues.
Common Causes of Lower Back and Pelvic Pain in Females
Lower back and pelvic pain in females can arise from a variety of factors, including musculoskeletal issues, hormonal changes, and reproductive health conditions. Conditions such as endometriosis, fibroids, and pelvic inflammatory disease can contribute significantly to this type of discomfort. Reproductive organs can be a source of lower back and pelvic pain. Conditions affecting these organs include endometriosis, where endometrial tissue grows outside the uterus, and fibroids, benign uterine tumours. Pelvic pain syndrome can also be related to pelvic organs and abdominal pain.
Injuries
Injuries to the lower back or pelvis, whether from accidents, sports, or falls, are a frequent cause of pain. These injuries can lead to muscle strains, ligament sprains, or fractures, resulting in localized pain and discomfort. Pelvic congestion syndrome, characterized by blood flow issues in the pelvic region, can cause chronic pain.
Muscle Strain or Overuse
Excessive physical activity or incorrect lifting techniques can strain the lower back and pelvic muscles. Overuse can lead to inflammation and muscle pain, making even routine activities challenging.
Bad Posture
Poor posture can contribute to lower back pain, especially when sitting for prolonged periods. Slouching or sitting with improper support can place undue stress on the spine and surrounding muscles, including the muscle wall.
Endometriosis
Endometriosis is a condition where tissue similar to the lining of the uterus, or endometrial tissue, grows outside it, often causing pelvic pain. This pain can radiate to the lower back, creating a complex pain pattern that affects many women.
Kidney Problems
Kidney infections or stones can cause referred pain in the lower back and pelvic area. Other symptoms, such as urinary issues or fever, often accompany this pain. Bladder pain syndrome may also be a factor.
Inguinal Hernias
An inguinal hernia occurs when part of the intestine protrudes through the abdominal wall or into the inguinal canal in the groin area. This can cause discomfort and pain in the lower abdomen and pelvic region, potentially affecting nearby nerves.
SI Joint Dysfunction
The sacroiliac (SI) joint connects the lower spine to the pelvis. Dysfunction or inflammation of this joint can lead to lower back and pelvic pain, affecting movement and stability. Facet joints can also contribute to this discomfort.
Degenerative Disc Disease
As we age, the discs between the vertebrae in the spine can degenerate, leading to pain in the lower back. Changes in spinal alignment can also affect the pelvic area. Spinal stenosis or an abnormal curvature may also be involved.
Arthritis
Arthritis, particularly osteoarthritis or rheumatoid arthritis, can affect the pelvis and lower back joints, causing pain and stiffness. This condition can limit mobility and impact daily activities. Connective tissues around these joints may be affected.
Pregnancy
Pregnancy brings about significant physical changes, including weight gain and hormonal shifts. These changes can strain the lower back and pelvis, leading to pain and discomfort. Vitamin D deficiency during pregnancy can also contribute to pain.
Menstrual Cramps
Many women experience pelvic pain due to menstrual cramps, which can sometimes extend to the lower back. This cyclical pain, often associated with painful periods, is usually managed with lifestyle changes and medication. Heavy periods and pain during sex can also be symptoms.
Scoliosis
Scoliosis, a condition in which the spine curves abnormally, can lead to uneven weight distribution and strain on the lower back and pelvis, resulting in chronic pain and discomfort. Scar tissue from previous injuries can exacerbate this issue.
Symptoms of Lower Back and Pelvic Pain
Pelvic and lower back pain symptoms can differ significantly based on the underlying cause. Common indicators include a dull or sharp ache in the lower back or pelvic region, pelvic pain walking that may radiate down to the legs or buttocks, stiffness accompanied by a restricted range of motion, and painful periods. Worldwide, the rates of chronic pelvic pain for women of childbearing age range from 14% to 32%. Between 13% and 32% of these women have pain that is severe enough to cause them to miss work.
How Are Lower Back and Pelvic Pain in Females Connected?
Lower back and pelvic pain often share a connection due to the proximity of the anatomical structures involved. The lower back and pelvis are interconnected through the spine, sacroiliac joints, and various muscles and ligaments. Issues in one area can often lead to pain in the other, creating a complex pain pattern that requires comprehensive evaluation and treatment.
Diagnosis of Lower Back and Pelvic Pain
Healthcare professionals will conduct a thorough medical history review and physical examination to diagnose pelvic pain and lower back pain. Imaging tests like X-rays or MRI scans may also identify underlying conditions or abnormalities. Physical symptoms vary widely, from neurological symptoms to abdominal wall trigger points.
Medical History and Physical Examination
A thorough medical history and physical examination are crucial in diagnosing the cause of lower back and pelvic pain. The healthcare provider will assess the patient’s symptoms, lifestyle, and any recent injuries or activities that might contribute to the pain. Family history of similar conditions may also be considered.
Imaging Tests
Imaging tests, such as X-rays, MRI, or CT scans, may be used to visualize the spine, pelvis, and surrounding structures. These tests can help identify issues such as herniated discs, fractures, or degenerative changes. Bowel movements and abdominal wall muscles might also be examined to rule out related conditions.
Lab Tests
Lab tests may be performed to rule out infections, inflammatory conditions, or other underlying health issues that could contribute to pelvic pain. Based on the symptoms and physical examination findings, blood tests, urinalysis, or other diagnostic tests may be recommended. Pain secondary to conditions like irritable bowel syndrome or neurological symptoms can be evaluated through these tests.
Treatment Options for Lower Back and Pelvic Pain in Females
There are various treatment options available for addressing lower back and pelvic pain in females, ranging from conservative therapies to more invasive procedures. These can include physical therapy, medications, lifestyle modifications, and, in some cases, surgical interventions, depending on the severity and underlying cause of the pain.
Non-invasive Methods:
Non-invasive methods for treating lower back and pelvic pain include physical therapy, which focuses on strengthening muscles and improving flexibility. Pelvic floor therapy Asheville NC can be particularly beneficial for addressing issues related to pelvic pain and dysfunction. Medications such as nonsteroidal anti-inflammatory drugs (NSAIDs) can also help alleviate pain and inflammation. Lifestyle modifications like weight management and regular exercise can significantly enhance recovery and prevent future pain episodes. Heating pads and muscle relaxants can also be useful for relief.
- Rest and Ice/Heat Therapy: Resting and applying ice or heat to the affected area can help reduce inflammation and alleviate pain. Alternating between ice and heat may provide additional relief. Belly pain can sometimes be managed with these methods as well.
- Over-the-Counter Pain Relievers: Pain relief and inflammation reduction can be effectively achieved with nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen or acetaminophen. These medications are commonly used to alleviate lower back and pelvic pain discomfort. Chiropractic care might also be considered for additional support.
- Physical Therapy: Physical therapy effectively strengthens the muscles that stabilize the lower back and pelvis while improving posture. This treatment approach can significantly enhance overall flexibility and mobility. Pelvic floor therapy can address issues with pelvic muscles and pelvic pain syndrome.
- Stretching and Strengthening Exercises: Targeted exercises can help relieve tension and strengthen the muscles around the lower back and pelvis. A physical therapist can design a personalized exercise program based on individual needs. Exercise may also target connective tissues and muscle pain relief.
- Massage: Therapeutic massage is beneficial for alleviating muscle tension and enhancing circulation. This treatment can effectively relieve discomfort associated with lower back and pelvic pain. Massage therapy may also help with pain in adult females.
Medical Intervention:
In cases where conservative treatments are insufficient, medical intervention may be necessary to address lower back and pelvic pain. This can include prescription medications, corticosteroid injections, or surgical options, depending on the underlying diagnosis and severity of the pain.
- Corticosteroid Injections: For more severe pain, corticosteroid injections can help reduce inflammation and provide temporary relief. These are typically used when other non-invasive methods have not been effective. Surgical treatment may be considered if necessary.
- Surgery (if necessary): In cases where conservative treatments do not provide relief, surgical treatment options may be considered. Surgery is usually a last resort and is only recommended after thorough evaluation and failed non-invasive treatments. Ovarian cancer or cervical cancer might also be assessed if relevant symptoms are present.
Prevention and Management Strategies
To prevent lower back and pelvic pain, it is essential to adopt healthy habits and lifestyle changes. Maintaining good posture while sitting, standing, and lifting can significantly reduce strain on the lower back and pelvis. Regular physical activity is crucial, strengthening core muscles and enhancing flexibility. Additionally, staying well-hydrated and consuming a balanced diet supports overall musculoskeletal health. Lastly, using proper lifting techniques, such as bending at the knees and keeping the back straight when handling heavy objects, can help minimize the risk of injury. Abdominal wall muscles should be strengthened to support this process.
When to Seek Medical Help for Lower Back and Pelvic Pain

It is important to seek medical assistance if you experience severe, persistent, or worsening pain. Additionally, you should consult a healthcare professional if your discomfort is accompanied by other concerning symptoms such as fever, unexpected weight loss, or alterations in bowel or urinary functions. A history of recent trauma or injury also warrants prompt evaluation. Abuse in women, such as sexual abuse or physical abuse, may also be relevant in some cases. Furthermore, if the pain significantly hinders your daily activities or diminishes your quality of life, seeking medical advice for proper diagnosis and treatment is crucial.
Conclusion
In females, lower back and pelvic pain can have various causes, ranging from muscle strain to underlying medical conditions. Understanding the potential causes and available treatment options is essential for effective management and relief. By taking a proactive approach to diagnosis, treatment, and prevention, individuals can improve their quality of life and reduce the impact of these conditions. Irritable bowel syndrome, neuropathic pain, and chronic disease should be considered in comprehensive care.
FAQ’S
What does it mean when your lower back and pelvic area hurts?
Pain in the lower back and pelvic area can result from various issues, including muscle strain, poor posture, or medical conditions like endometriosis or arthritis. Assessing the symptoms and seeking medical care to determine the exact cause is important.
How to relieve lower back and pelvic pain?
Relief can be achieved through various methods, including rest, ice or heat therapy, over-the-counter pain relievers, physical therapy, stretching exercises, and massage. In more severe cases, medical interventions such as corticosteroid injections or surgery may be necessary. Adjunctive therapy, like chiropractic care and floor physical therapy, may also be beneficial.
What can cause pelvic pain in a woman?
Pelvic pain in women can be caused by conditions such as endometriosis, menstrual cramps, pelvic inflammatory disease, ovarian cysts, or urinary tract infections. Other factors like pregnancy, pelvic congestion syndrome, or digestive disorders may also contribute to pelvic pain.